Helena Laroche, MD, FAAP, ABOM
Scientific Medical Director, Center for Children's Healthy Lifestyles & Nutrition; Associate Professor of Pediatrics, University of Missouri-Kansas City School of Medicine
Full Biography
When families struggle with social risk factors like inadequate housing or food insecurity, it impacts their health care. Helena Laroche, MD, FAAP, ABOM, Scientific Medical Director for the Center for Children's Healthy Lifestyles & Nutrition, researches the intersection between social risk factors and obesity prevention and treatment outcomes in the hopes of improving the lives of children and their families.
Social determinants of health
Social risk factor is another name for a negative social determinant of health. Social determinants of health fall into five categories: economic stability, education access and quality, health care access and quality, neighborhood and built environment, and social and community context. When families have trouble in any of those five categories, it’s considered a risk factor.
Much of Dr. Laroche’s research focuses on whether providing support to address social risk factors improves obesity treatment outcomes. In addition to her research, Dr. Laroche also works with children and their families in the Children’s Mercy Kansas City (CMKC) Weight Management Clinic.
NIH award to study social risk factors in obesity treatment
In May 2024, Dr. Laroche received a three-year, $819,130 R01 grant from the National Institutes of Health (NIH) to address social risk factors in obesity treatment. “The study combines family-based obesity treatment and working with community health workers to help hopefully mitigate at least a few of those social risk factors,” said Dr. Laroche. “Then, we look at whether that helps families do better in obesity treatment.” This project will determine the feasibility of a larger study in the future.
As part of this project, her team will look at the role parental bandwidth plays in successful treatment. Bandwidth is the ability to allocate and use limited cognitive resources effectively, and it is impacted by scarcity of time or resources. “You can only do so many things with your brain at one time, no matter who you are,” said Dr. Laroche. She explains how worrying about things like finding safe housing or paying for food takes up a lot of mental bandwidth. “If we could help by getting rid of a few of those worries and make something just a little bit better, we want to know if it will give people more space to focus on the things that they want to focus on, like their kids’ health,” she said.
If we could help by getting rid of a few of those worries and make something just a little bit better, we want to know if it will give people more space to focus on the things that they want to focus on, like their kids’ health.
The research team will recruit 60 families. All 60 families will complete a 12-week family-based lifestyle child obesity treatment program. Before completing the program, half of the families will work with community health workers to address social risk factors while the other half will receive one-time referrals to community organizations using resources from Lift Up KC, a database of community resources maintained by CMKC. Dr. Laroche partners with the Community Health Council of Wyandotte County (CHC) to provide community health workers for the project. CHC Program Director Katherine (Mariah) Chrans, PhD, IBCLC, is a co-investigator on the project and has been involved in the project since its inception.
The research team also includes CMKC co-investigators Andrea-Bradley Ewing, MPA, MA; Emily Hurley, PhD, MPH; Hung-Wen Yeh, PhD, MS; Jordon Carlson, PhD, MA; Sarah Hampl, MD; and Meredith Dreyer Gillette, PhD; and University of Kansas Medical Center co-investigators Debra Sullivan, PhD, RD, Laura Martin, PhD, and Ann Davis, PhD, MPH, ABPP. CMRI Community Advisory Board member Bruce Reed is a consultant on the project.
Mapping the referral process for community health workers
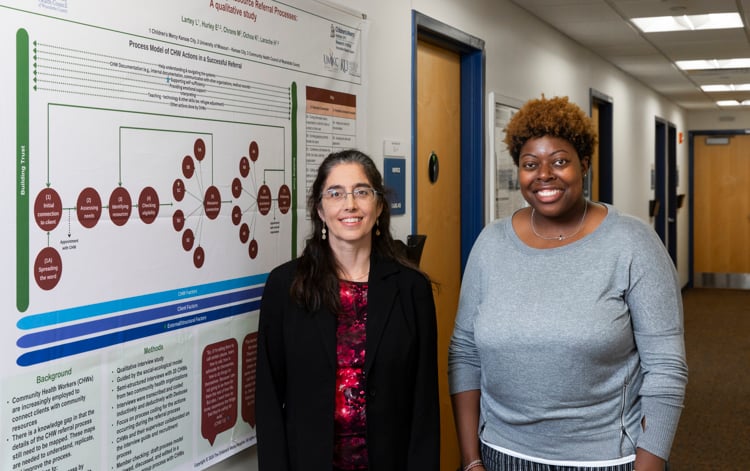
As Dr. Laroche collaborated with Dr. Chrans on the community health worker intervention for the NIH study, she wanted to better understand how community health workers do their jobs. To answer that question, she worked with Lynette Lartey, MPH, MCHES, and Dr. Hurley from the Formative Research team and Dr. Chrans and the CHC team of community health workers. “We want to understand how community health workers connect people with resources or referrals,” she said. “If we can understand that, then we can help make that process better. We can map out what the community health workers do.” The study team presented their research at the poster session of the 2023 American Public Health Association annual conference and the 2024 National Association of County and City Health Officials as well as some local conferences.
The client experience
Dr. Laroche also has another project that looks at the impact of addressing social risk factors from the client perspective. For this project, she works with Jannette Berkley-Patton, PhD, and her Healthy Jackson County grant. The research team asks people who participate in a diabetes prevention program about their experience connecting with needed resources and services. The program connects people with community health workers in Jackson County to get assistance or refers them to Lift Up KC.
“We want to make getting services easier,” said. Dr. Laroche. “To do that, we need to understand both what community health workers do and what the experiences of their clients are. Then, we can we tweak it to make it better, even if it’s the little things.”
Integrative Care Solutions
For another project, Dr. Laroche works with CMKC Integrated Care Solutions (ICS) to determine what interventions for social risk factors improve outcomes for patients. ICS coordinates medical care for pediatric patients throughout the region and includes CMKC employed pediatricians, pediatric specialists, and independent community pediatric providers.
ICS has increased its social risk factor screening for patients in its connected practices, and Dr. Laroche wants to determine if interventions to address those risk factors improved outcomes for the patients. “Some of the questions we want to ask are: What effect did it have on patients and outcomes for patients? What effect did it have on the pediatric practices? And which patients were screened and referred?” she said.
The study team is creating a baseline dataset pulled from a variety of data sources, including electronic health records, claims data and patient surveys. Going forward, they will follow patient data over time to study the relationship between interventions and patient outcomes. Dr. Laroche received a CMKC internal grant in October 2023 for the project.
The research team includes Michelle Manaskie, MPH, ICS; Nikita Sharma, MHA, ICS; Dr. Yeh, Health Services and Outcomes Research; and Jeffrey Colvin, MD, FAAP, Pediatrics.
Other research projects
Dr. Laroche is also collaborating with other CMKC researchers on an NIH-funded intervention to incorporate family-based obesity treatment into community health centers and on a CDC REACH grant expanding family-based obesity treatment availability in Kansas City. She is also site-principal investigator for an NIH clinical trial of phentermine, an appetite-suppression medication, in adolescents.
Looking to the future, Dr. Laroche would like to pull together what she learns about social risk factor interventions from all her research projects to improve the process to provide families with the resources they need. “I think that it could be built into any intervention that we do, but we need to do it right and we need to do it with the right partners in the community,” she said.
Full circle
Dr. Laroche’s interest in public health research traces back to her undergraduate days at Brown University. “I started out doing research as a sociology major and in public health before medical school, and then I circled back around to public health research,” she said.
After graduating from Brown, Dr. Laroche deferred medical school and worked on a project to improve the infant mortality rate in the Missouri Bootheel region. She received her MD from the University of Missouri School of Medicine in Columbia and completed her residency in internal medicine and pediatrics at the University of Rochester in New York. Dr. Laroche completed a Robert Wood Johnson Foundation Clinical Scholars Fellowship at the University of Michigan in Ann Arbor. “I was lucky enough to spend three years focusing on research while treating patients,” she said. “What I learn from working with patients informs what I do in the research setting and vice versa.” After the fellowship, she held an academic research position at the University of Iowa for 16 years, where she continued to focus on obesity research and practiced adult internal medicine.
What I learn from working with patients informs what I do in the research setting and vice versa.
Dr. Laroche joined Children’s Mercy in 2020 and is happy to work with children and families again. “Coming here allowed me to take my research to where it was headed,” she said. “I started out with an interest in obesity prevention, particularly community-based and family-based focuses, and working with low-income families. When I came here, I was surrounded by people doing similar work.”
In addition to her research and clinical roles at CMKC, Dr. Laroche is an associate professor at the University of Missouri-Kansas City School of Medicine.