Outbreaks, Alerts & Hot Topics: Mpox Redux
Column Author: Chris Day, MD | Director, Transplant Infectious Disease Services; Medical Director, Travel Medicine Program
Column Editor: Angela L. Myers, MD, MPH | Division Director, Infectious Diseases; Medical Director, Center for Wellbeing
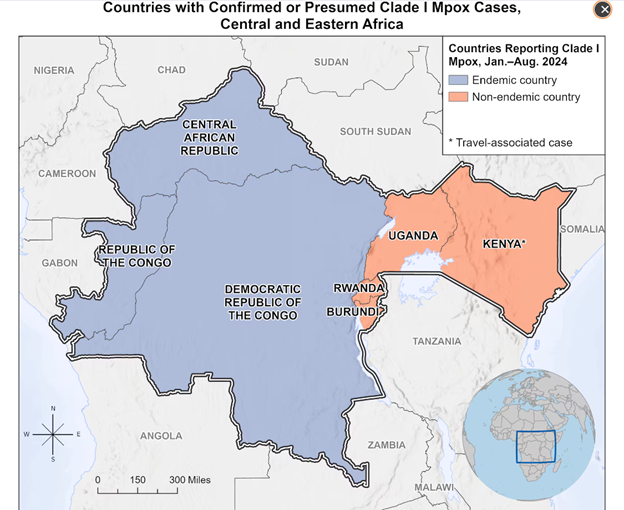
Worldwide human-to-human transmission of clade IIb mpox began in May 2022, with 95,000 global cases in 115 non-endemic countries documented so far.1 Later that year, widening interest in the infection resulted in a name change from monkeypox to mpox, prompted by the stigmatizing way the name was being used in some quarters.2 By May 2023, the World Health Organization (WHO) declared an end to the mpox public health emergency, though ongoing circulation of the infection continues, including in the United States. There is now a growing outbreak of a more deadly clade 1 mpox virus in the Democratic Republic of the Congo (DRC), prompting WHO to declare a Public Health Emergency of International Concern on Aug. 14, 2024. To date, this outbreak has caused 1,300 known deaths out of a 27,000 suspected mpox cases in the DRC, with additional cases in Central African Republic, Burundi, Rwanda and Uganda, as well as a few cases related to travel in Kenya (two), Sweden (one), and Thailand (one).3 In DRC, children under 15 have accounted for 67% of cases and 83% of deaths.4
Mpox is endemic to some populations of wild animals in DRC and several other African countries. Transmission appears to occur primarily through direct contact with lesions, but can also occur by way of fomites, possibly by droplet transmission, and vertically from mother to fetus. Current mpox transmission in DRC is from contact with wild animals, household contact, patient care, and sexual contacts including among men who have sex with men (MSM) and female sex workers and their contacts.3 Most cases in the ongoing United States clade IIb outbreak seem to be attributable to intimate contact.
According to the Centers for Disease Control and Prevention (CDC), the current risk posed by the clade I mpox outbreak to United States residents is low. However, the reasons behind size of the clade I mpox outbreak are not well understood and CDC reports a low confidence in this assessment (which they recently upgraded from a July assessment of very low risk). Current spread in some parts of DRC is primarily human-to-human. Should clade I mpox enter the U.S., risk in the United States from heterosexual sex is thought to be low, but there may be more potential for spread among MSM. The impact of this vulnerability might be reduced by immunity in the MSM population from prior infection and vaccination related to the clade IIb mpox outbreak.5
Pediatric mpox cases in the United States related to the 2022 clade IIb mpox outbreak have not been common: 125 cases were reported in 2022 among patients <18 years old, with 45 of those cases in children ≤12 years old. Most of these children were exposed through household contacts or caregivers.6
Clade I mpox appears to have a higher case fatality rate (CFR) and appears to cause more severe disease than clade IIb infection. DRC is currently reporting a CFR of 3%; however, this number may be high due to undercounting of cases in part related to insufficient resources for testing.5
Mpox lesions are firm or rubbery and often umbilicated. Fever, chills, malaise, myalgias and headache can occur either before or after lesions appear, or sometimes not at all. Some patients have sore throat, nasal congestion or cough. When mpox is suspected, PPE (personal protective equipment) including gowns, gloves, eye protection and N95 respirators are recommended. The diagnosis can be made using swabs for PCR. Specimen requirements will depend on the laboratory, but sharp instruments should not be used for collection or to unroof lesions.
Two vaccines may have some efficacy for preventing mpox, with JYNNEOS being the vaccine currently most used. Risk groups for which vaccination is recommended in the U.S. right now include MSM with high-risk behaviors and their sexual contacts, including teenagers. Alternatives for immunocompromised patients with an exposure who need preventive therapy may include vaccinia immune globulin and an antiviral, tecovirimat.
Antiviral therapy is also available for treatment of infected children, immunocompromised patients, patients with a variety of skin conditions (e.g., eczema, burns, impetigo), pregnant or lactating individuals, and those with ocular disease.7
Figure 1: Map (Source: CDC.gov)
References:
- Fact sheet: United States response to the clade I mpox outbreak in several African countries. News release. U.S. Centers for Disease Control and Prevention. August 22, 2024. https://www.cdc.gov/media/releases/2024/s0822-mpox-outbreak.html
- Damaso CR. Phasing out monkeypox: mpox is the new name for an old disease. Lancet Reg Health Am. 2023;17:100424. https://www.thelancet.com/journals/lanam/article/PIIS2667-193X(22)00241-1/fulltext
- Clade I mpox outbreak originating in Central Africa. Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of High-Consequence Pathogens and Pathology (DHCPP). Last reviewed September 6, 2024. https://www.cdc.gov/poxvirus/mpox/outbreak/2023-drc.html
- Mpox - Democratic Republic of the Congo. World Health Organization. June 14, 2024. https://www.who.int/emergencies/disease-outbreak-news/item/2024-DON522
- Mpox rapid risk assessment. U.S. Centers for Disease Control and Prevention. August 31, 2024. https://www.cdc.gov/cfa-qualitative-assessments/php/data-research/mpox-risk-assessment/index.html
- Nemechek K, Stefanos R, Miller EL, et al. Notes from the field: exposures to mpox among cases in children aged ≤12 years — United States, September 25–December 31, 2022. MMWR Morb Mortal Wkly Rep. 2023;72:633-635. doi:10.15585/mmwr.mm7223a4
- Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of High-Consequence Pathogens and Pathology (DHCPP). Last reviewed September 6, 2024. https://www.cdc.gov/poxvirus/mpox/index.html
