Pleural Fluid: What's the Diagnosis?
Visual Diagnosis - July 2023
Column Author: Chia-Chi Angela Fu | Pediatric Resident, PGY-3
Column Editor: Joe Julian, MD, MPHTM | Hospitalist, Internal Medicine-Pediatrics; Clinical Associate Professor, Internal Medicine & Pediatrics
A 14-year-old teenage boy presented with a one-day history of right ear pain and neck pain and stiffness. He reported associated headache, light sensitivity, and a few days of cough, congestion, and rhinorrhea but no sore throat. There were no fevers, chills, night sweats or weight loss. He denied any dyspnea on exertion, chest pain or decrease in activity. He denied any recent trauma. He was otherwise healthy, and the family history was notable only for lupus in patient’s mother and hypertension in patient’s father. Immunizations were reported to be up to date.
Vital signs were within normal for age. On exam there was swelling to the right posterior auricular area extending down to the nape without overlying erythema of the skin. Conjunctival and oropharyngeal examinations were unremarkable. There were diminished breath sounds over the left lung fields. The cardiac examination was unremarkable.
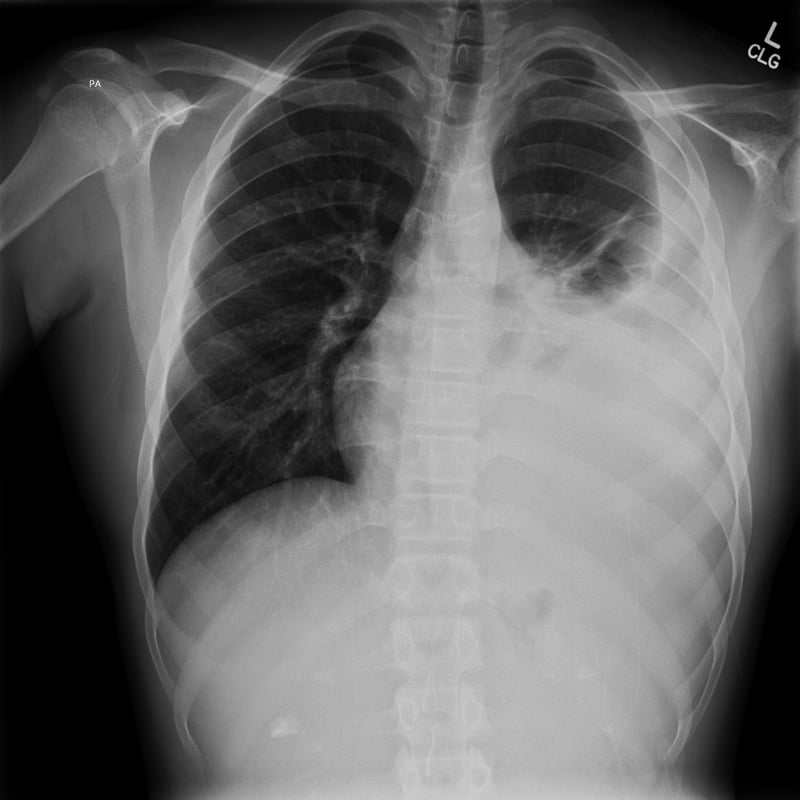
Initial work-up consisted of contrasted computed tomography (CT) of the head and neck, which revealed a filling defect within right transverse sinus, sigmoid sinus and internal jugular vein suggestive of venous thrombosis. Chest x-ray revealed the following below:

The patient was admitted, and the next morning a chest tube was placed.
Which of the following pleural fluid findings is most likely?
- Transudative fluid, consistent with new-onset heart failure
- Exudative fluid, consistent with rheumatologic disease
- Transudative fluid, consistent with malignant process
- Hemorrhagic fluid, consistent with hemothorax
- Exudative fluid, consistent with infection
Answer: B. Exudative fluid, consistent with rheumatologic disease
The above case scenario has a few important “buzz words” which prompted admission and early intervention:
- The patient was a young adolescent male.
- Unilateral ear/neck pain after a few days of upper respiratory infection symptoms.
- Notable physical exam findings of asymmetric auricular/neck region.
- CT findings suggestive of thrombosis.
- Chest x-ray findings consistent with pleural effusion so large that it cannot exclude pneumonia.
Extended history taking revealed a strong familial history of systemic lupus erythematosus (SLE). SLE is a widely known autoimmune disease with complex poorly understood pathophysiology and a variety of manifestations. The primary pathologic findings of SLE include inflammation, vasculitis, immune complex deposition and vasculopathy. Initially used to describe skin lesions, “systemic” was added to the name given the systemic characteristics of the disease, involving several organs – brain, blood and kidney, to name a few.
The patient did not have any symptoms of heart failure (decreased activity, dyspnea on exertion) or trauma (specifically to the chest), which goes against heart failure or hemothorax as etiologies of the pleural fluid. Malignancy is less likely as there are no other concerning symptoms such as night sweats or weight loss. Also, pleural effusions related to malignancy are almost exclusively exudate which makes this specific answer unlikely.
The physicians caring for this patient had concern for Lemierre’s disease. This condition is a result of bacteria, most commonly Fusobacterium necrophorum, invading the pharyngeal mucosa and lateral pharyngeal space. This infection and inflammation results in internal jugular vein septic thrombophlebitis and metastatic lesions, most commonly pneumonia or pleural empyema. The key to diagnose this disease is high clinical suspicion. These patients generally present with fever, severe sore throat, oropharyngeal findings on examination, and neck swelling with pain. However, it is important to note that some of the above findings are not exclusive to infectious processes as noted in this scenario.
Lung involvement is the most affected area of Lemierre’s disease, due to hematogenous spread. These lesions can develop into necrotic cavitary lesions, pleural effusions, empyema, lung abscesses and necrotizing mediastinitis. There are also a variety of presentations of lung involvement in SLE: lupus pleuritis, pleural effusion, acute lupus pneumonitis, shrinking lung syndrome, interstitial lung disease, diffuse alveolar hemorrhage, pulmonary arterial hypertension and pulmonary embolism. Via biopsy, it has been identified that pleural involvement shows lymphocytic and plasma cell infiltration. With these two disease processes having similar presentations, it becomes difficult to distinguish between the two which have very different treatments.
In this case, the below findings are from the pleural fluid obtained at time of chest tube placement. In adults, the type of effusion (exudative vs. transudative) is determined by Light’s criteria, which compare both total protein and lactate dehydrogenase (LDH) in serum and pleural fluid. Meeting any one of the following is considered an exudative effusion: (1) pleural fluid protein / serum protein >0.5, (2) pleural fluid LDH / serum LDH >0.6, or (3) pleural LDH > 2/3 upper limit of normal for serum LDH. While extrapolated from adult literature, there is evidence to support the use of Light’s criteria in the pediatric population (especially in unclear etiologies).3
Serum LDH 685 (upper limit ~200 in teens)
Serum Glucose 89
Serum Protein 6.8
Pleural fluid LDH 721
Pleural fluid Glucose 82
Pleural fluid Protein 4900
Cell count:
RBC <2000
WBC 431 (55% lymphocytes, 26% neutrophils, 14% macrophages, 5% eosinophils)
CALCULATIONS:
(1) pleural/serum protein = 720
(2) pleural/serum LDH = 1.1
(3) pleural LDH 721 > 2/3 upper limit of 200
Using Light’s criteria, it is clear the pleural fluid is exudative by all three measures. Interestingly, the identification of the total nucleated cell count reveals mostly lymphocytes, seen in the disease process of SLE as discussed. In the setting of infection causing empyema, a neutrophil predominance is found. It is also important to note that the red blood cell count, although high, does not meet the definition of hemorrhagic effusion (<100,000).
On admission, the patient promptly received antibiotics due to the concern for Lemierre’s disease while infectious studies were pending. Given the family history of SLE, several rheumatologic studies were also sent out early during hospitalization; they confirmed the diagnosis of SLE. Several factors played into the decision of continuing antibiotics vs. stopping them completely as the patient needed to start immunotherapy for SLE. By time of discharge, the patient had completed a course of antibiotic therapy, received anticoagulation, and completed a course of burst steroids with a plan to continue parenteral and oral immunotherapy.
References:
- Lee WS, Jean SS, Chen FL, Hsieh SM, Hsueh PR. Lemierre’s syndrome: a forgotten and re-emerging infection. J Microbiol Immunol Infect. 2020;53(4):513-517. doi:10.1016/j.jmii.2020.03.027
- Shin JI, Lee KH, Park S, et al. Systemic lupus erythematosus and lung involvement: a comprehensive review. J Clin Med. 2022;11(22):6714. doi:10.3390/jcm11226714
- McGraw MD, Robison K, Kupfer O, Brinton JT, Stillwell PC. The use of Light’s criteria in hospitalized children with a pleural effusion of unknown etiology. Pediatr Pulmonol. 2018;53(8):1101-1106.
See all the articles in this month's Link Newsletter
Stay up-to-date on the latest developments and innovations in pediatric care – read the July issue of The Link.